Speech Therapy
If you and others are having a difficulty time understanding what your child is saying and they are demonstrating speech sound errors, your child likely has an articulation or phonological disorder. Don’t let the long names or the word “disorder” intimidate you! These are simply referring to the intelligibility (or clarity) of your child’s speech and can be remediated by a speech-language pathologist. Here is a great chart to follow:
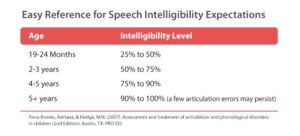
If your child is producing some speech sound errors beyond what is typical for their developmental age, and are considered “mildy” unintelligible, it is likely an articulation disorder.
Articulation Disorder- strategies for home carryover
1) Practice your child’s speech sound being targeted in therapy in a mirror!

2) Practice your child’s speech sound in a book! This will increase their awareness of the targeted sound. Find books from your local library that have repetitive words with the appropriate speech sounds to target. (For example, if the sound is /g/, try “Go Dog GO!” by P.D. Eastman)

3) Draw attention to your mouth while speaking and use cues to your mouth so that the child can follow your cues for correct speech production on the targeted sounds.

If your child is “highly” unintelligible due to an excessive use of phonological processes that are typical for development, then it is likely a phonological disorder. Please refer to the phonological processes chart from the American-Speech and Hearing Association (ASHA) here: https://www.asha.org/Practice-Portal/Clinical-Topics/Speech-Sound-Disorders-Articulation-and-Phonology/Selected-Phonological-Processes/
Phonological Disorder- strategies for home carryover
1) If your child is deleting final speech sounds in words, make a “snake” down your arm with your pointer finger and “stop” the snake to mark the final speech sound.

2) To increase awareness of speech sounds, hide your mouth using a small piece of paper and say a targeted word (with the speech sound targeted) correctly and correctly to see if your child can hear the difference and ask them to give you a “thumbs up!” or “thumbs down” to that word with the speech sound. (pic as follows) For example, say “ship” and “sip” if the child is having a difficult time producing the /s/.

3) Minimal pair practice- using rhyming words that have the initial speech sound being substituted with the appropriate production. For example, if a child is producing the s/z, you would have the child say “sip” and “zip” or “sap” and “zap” so they can feel the difference of productions and increase their awareness of productions and practice the sounds.
At ABC, our ASHA certified and licensed speech-language pathologists can help remediate speech sound errors. Learning through play is crucial to your child’s development and we provide a sensory-enriched experience to allow for kids to target their speech sounds in a fun, play-based approach! Please visit our website https://www.abcpediatrictherapy.com for answers to your questions.
Read MoreHolidays are a fun and exciting time of the year. Holidays can also be a stressful time of the year for both children and their parents. Children with deficits with sensory processing may have more difficulty with maintaining appropriate modulation which may lead to being overwhelmed and having more melt-downs. Keeping in mind the following strategies can help families get though the holiday season with less frustration.
· Put up Holiday decorations slowly over time. Allow your child to be part of the process of decorating so that she does not get overwhelmed with the lights, sounds, or changes in furniture set up.
· If you take your child shopping with you, try to avoid shopping at crowded or busy times. Shopping ahead of time or online might be appropriate alternatives.
· Educate extended family members about your child’s difficulties with sensory processing and let them know if there are any changes and adaptations that you will be making to traditional Holiday get togethers.
· When going to outings that may be overwhelming take your child’s comfort items and familiar toys for him to play with.
· Let your child know ahead of time what activities are scheduled. Let them know what the activity is, when it will take place, and what to expect. If possible, it may be beneficial to create a social story with pictures from previous years if possible to share with your child before an event.
· Try to stay on your normal routine: Try to be consistent with wake-up times, nap times, meal times, and bed times. Try to keep the same bedtime routine allowing time for your child to calm down before bed.

· Allow for extra rest and nap times if needed. Schedule in times for your child to have down time from scheduled activities in a quieter place.
· When going to family meals: allow for your child to eat at their typical meal time. Bring food that your child will usually eat and allow them to eat the familiar foods.
· When going to relatives/friends’ houses for get togethers it may be helpful to talk to the host a head of time to see if there is a separate place for your child to go to calm down if needed or to warm up to transition to environment.
· Dress your child in comfortable and familiar clothes. Allow the child to wear his favorite pants with a Holiday shirt, looks for clothes in the same fabric that they are used to wearing. For Holiday outfits, allow the child to wear the outfits before a holiday gathering.
· Be flexible on your expectations for traditional holiday activities. Allow for your child to stand near Santa or give him a high-5 instead of having your child sit on Santa’s lap for a photo. Let a child open only one or two gifts at a get-together and take the remaining gifts home to open at a later time.
Check out our video: Preparing your sensory child for a Holiday – YouTube
Staying flexible and making small adaptations can help you and your child have a more enjoyable Holiday season. For more information about sensory processing and development milestones please visit our website at: www.abcpediatrictherapy.com
Read MoreASAP, YMCA, RSVP. Acronyms are all around us, permeating our lives and activities. Sometimes we truncate words just for the heck of it, “kay” instead of “okay” or “app” instead of application. Then there’s the world of healthcare and medicine, and suddenly everything is a jumbled mess of alphabet soup. It’s hard to keep track of what all the acronyms and abbreviations stand for, so today’s focus is on AAC. It stands for Augmentative and Alternative Communication.
That’s a lot of words and letters to type; healthcare professions like the quick version “AAC” much better. As parents, it’s a lot scarier to hear another clump of letters without really understanding what it means. AAC is basically a way for individuals to get help (augment) or replace (alternative) communicatio n. AAC can come in a high tech form or a low tech form.
n. AAC can come in a high tech form or a low tech form.
Low tech AAC is anything that doesn’t get programmed with a digital voice, message, or screen. There is a low tech form of AAC called Picture Exchange Communication System (sorry, it’s another acronym: PECS), which is all about requesting and then commenting using special pictures. Other low tech forms of AAC could be a book full of pictures people can point to for requesting or even a book of common people or activities in their day-to-day life. High tech AAC (think Stephen Hawkings) is about ease of access, comfort of use, and typically is used by communicators with a little more ability to understand the complexity of a more complicated system, although preschoolers to the elderly can use high or low tech AAC.
High tech AAC can be as simple as one giant, clicking button, called a switch. Some switches have 1 big button, others have a few smaller buttons. Each button holds a single, recorded message. When the communicator bumps or hits the switch, the message plays. AAC can also be as complicated as an IPad application or specialized, portable machine that’s only job is to talk. These higher tech devices come with programmed software from screen layouts of 4 to 50 full of vocabularies, subjects, word prediction, keyboards, games, search functions, access to the internet for social networking, and the list of possibilities goes on.
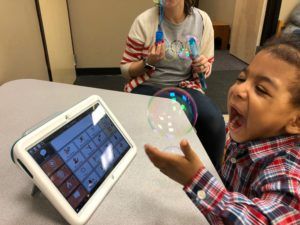
Now that we’ve had a quick background, the initial fear of the unknown should be fading…and all the questions are forming. The first thing to realize is that AAC can either augment language where it boosts, helps, and lifts a speaker’s verbal communication or it can be an alternative for them, or the third option: AAC can do both augment and be an alternative. Simply because a kiddo needs AAC doesn’t mean they don’t need their voice. Having goals in therapy to address AAC doesn’t mean your child isn’t learning to use their verbal words. In no way does it mean a child’s verbal and expressive language skills will fade, stop, or never grow. In fact, the truth is that AAC does the opposite. It makes verbal language explode. AAC gives children with a variety of diagnoses, disorders, delays, and deficits the ability to communicate with adults, teachers, and peers who may not have understood them before. It teaches children to actively seek out communication partners, to make requests, and to share their thoughts and ideas in a way that without the AAC would likely not have happened. AAC gives children opportunities. AAC gives children confidence. AAC gives children power. AAC gives children models, repetitions, and examples of more words than they would have had access to on their own, and soon, the children have heard the word enough from the AAC, that they can start verbalizing it on their own. AAC is fully customizable, modifiable, and portable. It goes where your child goes, can be used as your individual child needs, and there is no limit to the potential for their language. AAC is kind of like pixie dust…a little sprinkle can transport a child to Never Neverland: a new world of wishes, wonder, and words that they’ve never, never seen before…and you get to go along for the ride.
Read MoreAre you having trouble motivating your child to practice their speech and language skills at home? Your child’s speech therapist is likely assigning tasks to practice at home throughout the week to reinforce the skills they’re learning in therapy. Home practice can make a huge difference in their progress and usually means faster improvement. Speech therapy isn’t an easy fix and it requires a lot of hard work and consistent practice over many months or even years. Home practice does not have to be boring! Below is a list of applications, websites, and games that you can utilize to make home practice fun:
- Applications

o My PlayHome
- Compatibility: iPhone, iPad, and iPod touch
- Price: $3.99
- Description: My PlayHome is an interactive doll house game that contains a variety of male and female characters that can eat, drink, cook, shower, sleep, and so much more. Your child can explore every room in the house while enjoying the colorful and detailed illustrations.
- How to use it:
- Expressive language skills: Labeling actions and common objects, producing regular and irregular past tense verbs, answering wh- questions, describing picture scenes, telling how common objects are used, naming categories, producing he/she pronouns and regular plural -s.
- Receptive language skills: Identifying common items, understanding verbs in context, understanding use of common objects, following directions, and understanding pronouns.
- Why it works: My patients absolutely love this game. It is so fun and motivating- they don’t even realize they are working on a variety of language skills!
o Articulation Station
- Compatibility: iPhone, iPad, and iPod touch
- Price: Lite version is free, individual sounds range from $3.99 to $7.99, and full version is $59.99
- Description: The application includes 22 different sounds and 6 engaging articulation activities to help your child speak and pronounce their sounds more clearly.
- How to use it: Select the individual sound(s) your child is working on in speech therapy and practice at the word, phrase, sentence, or story level.
- Why it works: The application is fun, colorful, and engaging. You can practice your child’s sounds through flashcards, matching games, rotating sentences, unique sentences, and stories. The activities are so fun that my patients often forget they are “working” on their articulation skills.
- Websites
o Home Speech Home
- Link: https://www.home-speech-home.com/
- Description: Home Speech Home is a website created by two certified speech-language pathologists. This website offers a variety of activities and word lists to practice articulation, apraxia, language, and stuttering principles. In addition, speech and language developmental norms and an overview of various speech and language disorders are also included.
- How to use it: I frequently utilize the word lists feature with my older patients. I select the specific sound(s) that my patient is working on and incorporate the words while playing their favorite board game or within conversation. You can practice their articulation skills at home with premade words, phrases, sentences, and stories.
o Mommy Speech Therapy
- Link: http://mommyspeechtherapy.com/
- Description: Mommy Speech Therapy is a website created by a certified speech-language pathologist. This website offers a variety of free articulation worksheets that include colorful pictures of your child’s specific target words, as well as helpful tips and tricks on how to increase your child’s speech and language skills at home.
- How to use it: You can select your child’s specific sound(s) and print out the associated free articulation pictures, cut them into individual pictures, and play a variety of games at home. You can hide the pictures around the house and have a “scavenger hunt” and ask your child to name the pictures when they find them. You can print out an extra page and play Go Fish or a matching game with the pictures while reinforcing their articulation skills. The options are limitless!
- Games

o Guess Who
- How to play: You can target a variety of language and articulation skills with this classic board game. Guess Who is great for working on he/she pronouns, asking questions, answering yes/no questions, producing grammatical forms (e.g. do/does, has/have), and articulation skills at the conversational level.
o Hedbanz
- How to play: Hedbanz is a fun way to work on naming categories, answering yes/no questions, turn taking, and articulation skills while your child guesses the identity of the card they’ve been dealt.
o Simon Says
- How to play: Simon Says is a quick and easy game to work on identifying common objects (e.g. body parts), following one-step directions, as well as directions of increasing length and complexity.
If you have questions about your child’s speech and language skills please contact ABC Pediatric Therapy Network at https://www.abcpediatrictherapy.com.
Read More
Medical Model
In the medical model, an occupational, physical, or speech therapist performs evaluations and treatments in a clinical setting after being referred by a doctor. These evaluations and treatments often mimic a child’s natural play environment. Therapists look at the whole child, and their ability to function in all aspects of daily life. Goals are focused toward the child’s home and community function, as opposed to their function at school. However, the interventions at school and in the clinic may go hand in hand. For instance, if a child needs to improve balance and strength in order to get to downstairs at their school, they will also need to improve balance and strength to climb up the stairs at home to get to their bedroom. 
ABC Pediatric Therapy Network (www.abcpediatrictherapy.com) has six locations throughout the Cincinnati and Dayton areas that present children with the challenges of their home and community environment. All locations have a full-size jungle gym, trampoline, and foam pit in the large gym setting. For example, the foam pit can be used in therapeutic ways to help a child to gain motor planning through building block towers, and to gain coordination, trunk strength and upper extremity strength through swinging. As treatment is completed on the equipment, children are able to gain confidence in themselves, which will carry over to the playground and school. This will allow the children to better interact with peers in the classroom and playground.
In the clinical setting, therapists interact not only with the child, but also with the child’s primary caregiver, and siblings. Family dynamics are taken into consideration when forming a treatment plan that is realistic to the child and family as a whole. Families are an active participant in therapy sessions, and help form goals that would be beneficial to the child’s function throughout the day. ABC Pediatric Therapy Network also understands the importance of peer interaction and encourages patients to interact with each other during treatment. This allows children to build social skills such as initiating conversations, turn taking, and sharing. Children will often play games together to work on social skills including conversational skills, and appropriate responses to winning and losing.

Occupational, physical, and speech therapists working in a clinical setting offer direct, individualized treatment to their patients. At ABC Pediatric Therapy Network, therapists are part of a unique multidisciplinary team. This is a major benefit to the patients because skills that are being targeted during one therapy can be enforced during the other therapies. For instance, if the speech therapist is working toward a goal of a child using three-word requests, the physical therapist can augment his or her treatment by having the child use a three-word request prior to carrying out the activity (i.e. “kick the ball”).
School-based therapy uses an educational model that focuses on academic performance, and is governed by IDEA (Individuals with Disabilities Education Act). In the educational model, children with disabilities benefit from evaluations and treatments in a setting that is in their natural environment with their peer group. This model of pediatric therapy also focuses on a multidisciplinary approach to the therapy assessment, planning, and intervention. A multidisciplinary team includes the parents, teacher, special education teacher, and therapists. The team must be in agreement in order to implement an Individualized Education Plan. In order to receive therapy services at school, a child’s functional performance must be impaired to the extent that it interferes with the child’s functioning at school. Each district has strict standards for qualifying children for an Individualized Education Plan. The emphasis of treatment is on function at school and goals are related to the educational program. The therapy intervention may be direct, indirect, or on a consultation basis. Therapy is often in a group setting rather than an individual one-on-one session.
Therapists also make significant contributions to school programs by identifying environmental barriers and planning for accessibility modifications. They adapt classrooms to provide the optimal learning environment for children with special needs, help promote acceptance of students with disabilities, adapt recreational activities, and contribute to the development of safety procedures for emergency evacuation of students with disabilities. Occupational therapists may help include modifications and accommodations in the classroom including sensory seating, break areas, or specialized fine motor tools. Speech therapists may help in making visuals including communication picture books, break cards, or visual schedules to help ease transitions and communication in the school environment.
In the end, it all about progress. Is your child making the progress you want to see? If so, fantastic! Do not change a thing! If not, look for additional help to ensure your child reaches his/her maximum potential. Delays in development can effect self esteem, the ability to make friend and academic performance. Let’s work together to help every child to succeed!
If you have questions about next steps for your child, please go to www.abcpediatrictherapy.com or give us a call at 513-755-6600.
Read MoreWhen is it “appropriate”
Many young children go through periods of times where their speech is “disfluent”, or bumpy-sounding. These bumpy periods often occur during “language explosions” when children are rapidly learning new words and grammatical structures. Your child’s disfluencies may be developmentally appropriate if he or she:
· occasionally repeats the first sounds or word in a phrase (usually 1-2x)
· is between the ages of 1.5-5 years old
· has disfluencies that are not consistent; your child may go through phases of disfluency that go away on their own after a short period of time
When to seek help from a therapist
There are several red flags that indicate a child’s disfluencies may be indicative of a “true stutter” vs. developmental disfluencies. You should consider having your child evaluated by an ASHA certified speech-language pathologist if one or more of the following red flags are present:
· your child’s disfluencies have lasted for longer than 6 months
· your child is 5 years old or older
· you have a history of stuttering in your family
· your child is a boy (boys have been shown to stutter 4x more than girls)
· your child’s disfluencies occur more frequently/appear more severe
· your child gets “stuck” on sounds or words, typically at the beginning of sentences and phrases, and can’t “get their words out”
· your child may prolong sounds, such as “mmmmmmmmore please”
· your child’s dysfluencies appear effortful and strained
· your child demonstrates “secondary characteristics”, or behaviors that occur during disfluencies, i.e. forcefully blinking eyes, slapping leg, turning away
· your child is aware of their disfluencies and becomes upset, embarrassed, or frustrated when disfluencies occur
Can you prevent stuttering?
Unfortunately, there are no known ways to “prevent” your child from developing a stutter. Stuttering is a neurological communication disorder that can be “caused” by a combination of complex factors, including genetics, child development, neurophysiology, and family dynamics. (see FAQ from The Stuttering Foundation website). There is currently no known “cure” for stuttering; however, there are many treatment approaches that can be performed by a speech-language pathologist that have been proven affective in helping to reduce or eliminate stuttering. There are also many ways that you can change the way you and your child communicate to promote smooth, more fluent speech in the home- see the parent section below for tips and tricks for increasing your child’s fluency.
How to treat stuttering
There are a variety of treatment methods to help reduce the frequency of stuttering and promote smooth speech. A speech-language pathologist can help determine the severity and types of dysfluencies that your child is experiencing and will assist in developing a plan of treatment that is best suited for your child. This plan of treatment may include modification of speaking rate, modification of muscle tension/relaxation during speech, modification of respiration, etc. A speech-language pathologist will also work with your child to help them learn more about stuttering and its causes, as well as helping your child identify any negative emotions associated with stuttering and working through these emotions to achieve fluent speech. For more detailed information regarding treatments for stuttering, please visit the American Speech-Language-Hearing Association website.
How a parent can help at home
You can help your child reduce his or her dysfluencies at home in the following ways:
· Slow it down! Model slow and relaxed speech around your home. This helps reduce the “pressure” your child may feel to “keep up” by using fast paced speech, which often leads to increased disfluencies
· Make time for your child to communicate with you. Set aside a time of the day where you can listen to your child without multi-tasking or interjecting with questions or comments- allow your child to tell you whatever they’d like without feeling any pressure.
· Before responding to your child or other family members, try to pause rather than immediately responding. This encourages a more relaxed pace for communication for the whole family
· Don’t interrupt or try to “finish” a sentence for your child when they are stuttering- this can be discouraging for your child and make them feel that they have failed in their attempt to communicate. Allow them to finish their thought regardless of the length of stutter. Try to avoid speaking about or reacting in a negative way when stuttering occurs; reacting in a kind and accepting way can help encourage your child.
What can happen if stuttering goes untreated
If stuttering remains untreated, it can have serious emotional consequences for your child as they grow older. Children who stutter often experience negative emotions associated with their stuttering, including feelings of frustration, anger, confusion, embarrassment, and sadness. Children who stutter may start to withdraw socially. They may experience anxiety in social situations and “pressured” communication settings, such as restaurants, stores, etc. You child may have difficulty participating in school activities or being in front of others during presentations or speeches. Treatment of stuttering by a certified speech-language pathologist can not only help your child become more fluent, but can also help your child understand and confront the negative emotions associated with stuttering. As stated by the Stuttering Foundation, “Overcoming stuttering is often more a matter of losing fear of stuttering than a matter of trying harder”; a speech language pathologist can help assist you and your child on your journey to reduce stuttering.
If you have questions or concerns regarding your child’s fluency, please see the ABC Pediatric Therapy Website, www.abcpediatrictherapy.com, for more detailed information or call any of our locations to speak with a speech-language pathologist.
Read MoreIf your child has a speech disorder, he or she might be able to qualify for financial aid. The Social Security Administration (SSA) offers disability benefits to people of all ages who are unable to work, or in your child’s case, participate in typical childhood activities due to a disability. Speech disorders alone will not qualify, but depending on the cause of your child’s speech disorder, he or she may be eligible.
Technically Qualifying for Social Security
All children are eligible for Supplemental Security Income, or SSI benefits. SSI is only awarded to families with a severe financial need. This means that if you or your spouse earns a decent wage, you will not be eligible for disability benefits. The larger your family, the higher your monthly income limit will be.
For example, if you’re a single parent and you have one child, you cannot earn more than $38,000 before taxes in 2018 and still qualify for SSI. If you are a two-parent household of five, you could earn a little over $55,000 and still qualify. You can view a chart on the SSA’s website to determine how much your unique family could make while still qualifying.
Unfortunately, most children are denied SSI benefits due to household income limits. The good news is once your child turns 18, your income will no longer against your child, even if he or she still lives at home.
Medically Qualifying With a Speech Impairment
All conditions that qualify for disability benefits can be found in the Blue Book, the SSA’s manual of qualification criteria. There is a separate version of the Blue Book for both children and adults. Children do not qualify for a speech disorder alone, so this means that if your child has no other diagnoses or disabilities, he or she will unfortunately not qualify for disability benefits due to an inability to speak.
If your child’s speech impairment is cause by another condition, he or she may be eligible. There are many qualifying conditions listed in the Blue Book, but some conditions that often qualify include:
Autism
Autism can be found in Section 112.10 of the Blue Book. Under this listing, your child will qualify if he or she has measurable difficulty in any form of communication (verbal, nonverbal, social interaction) and has severely limited interests or participates in repetitive patterns of behavior. Children with autism will also need to have medical evidence proving severe difficulty with one of the following areas of physical functioning:
- Understanding and remembering information
- Interacting with others (playing with children, following adults’ instructions)
- Concentrating and accomplishing tasks
- “Adapting oneself,” which means controlling emotions in a school setting
Down syndrome, on the other hand, will automatically medically qualify with a karyotype analysis. The only exception is if your child has Mosaic Down syndrome (2% of the Down syndrome population), which often has less severe health and intellectual complications will need a little more medical evidence.
The en tire Blue Book can be found online so you can review the listings with your pediatrician to see if your child qualifies.
tire Blue Book can be found online so you can review the listings with your pediatrician to see if your child qualifies.
Starting Your Application
Before applying, you should always review the Child Disability Starter Kit to get a list of all documents needed before officially applying. You’ll have to apply for SSI benefits in person at your local SSA office. Your child does not have to be present for the application process. To schedule an appointment to apply in person, call the SSA toll free at 1-800-772-1213.
Helpful Resources:
Household SSI Limits: https://www.ssa.gov/ssi/text-child-ussi.htm
Childhood Blue Book: https://www.ssa.gov/disability/professionals/bluebook/ChildhoodListings.htm?PHPSESSID=2e1852cec574b204c1062189dbe882f2
Local SSA Office: https://www.disability-benefits-help.org/social-security-disability-locations
Child Disability Starter Kit: https://www.ssa.gov/disability/disability_starter_kits_child_eng.htm
Provided to ABC Pediatric Therapy Network, https://www.abcpediatrictherapy.com by:
Deanna Power
Director of Outreach
Disability Benefits Help
Read More Skip to content
Skip to content