Treatment for ADHD Learning Disabilities
What is Attention Deficit Hyperactivity Disorder (ADHD)?
Attention Deficit Hyperactivity Disorder also known as ADHD is a common brain disorder often diagnosed in childhood and lasting into adulthood. Individuals with ADHD typically have trouble paying attention, controlling impulses, and demonstrate excessive activity.
ADHD typically have trouble paying attention, controlling impulses, and demonstrate excessive activity.
What Are Common Signs of ADHD?
Children with ADHD often present with difficulties with attention, impulsiveness, and hyperactivity. They may also demonstrate challenges with attentional and cognitive skills such as problem-solving, planning, sustained attention, working memory, and cognitive flexibility. Children with ADHD often have problems with emotional regulation and may become more easily upset when things do not go their way or when they cannot get what they want right away often leading to difficulty with social interactions.
How is ADHD Diagnosed?
There is no single test for diagnosing ADHD. Diagnosing ADHD usually consists of a physical examination that consists of vision and hearing testing to rule out other problems that may present similarly to ADHD. The process may also include reports about the child’s behavior in a variety of setting from the parents, teachers, and sometimes the child and a checklist to rate ADHD symptoms. ADHD is diagnosed if the child demonstrates a persistent pattern of inattention and/or hyper activity that affects their functioning or development.
How is ADHD Treated?
ADHD is typically treated with a combination of treatment strategies. Treatment often includes a combination of medication, behavior therapy, occupational therapy for the child and education and training for parents and families.
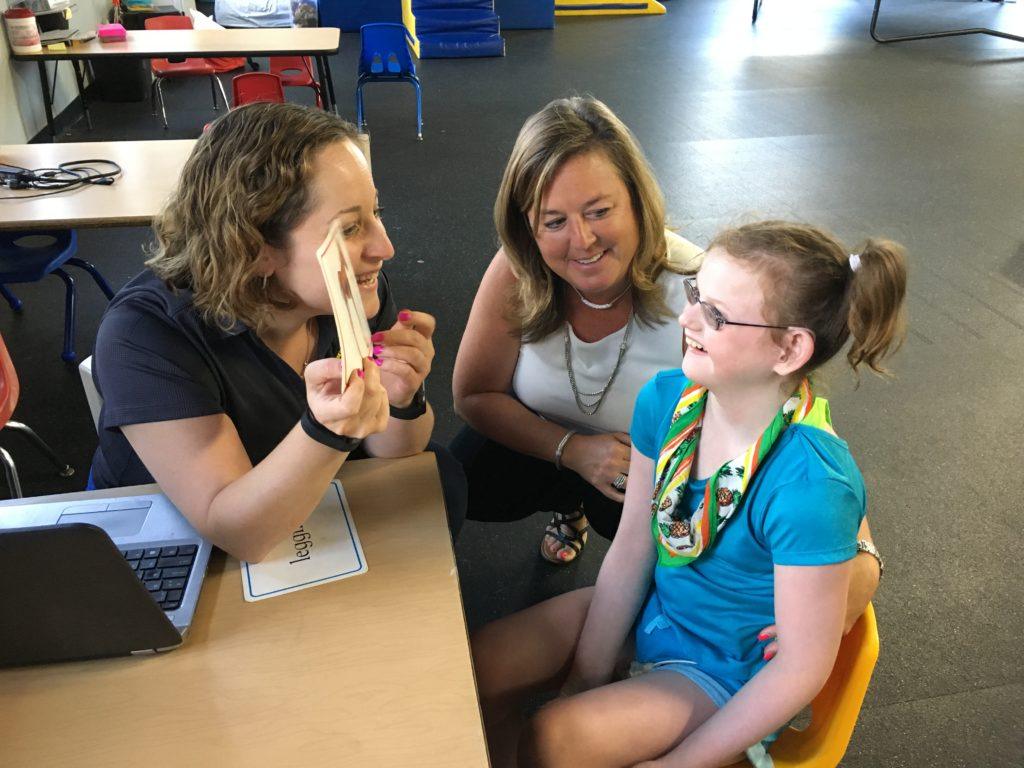
Occupational Therapists at ABC teach children strategies to improve focus, learning/study skills, social skills that leads to the ability to make friends and emotional self regulation.
For children under 5, behavior therapy and parent education are typically the first strategy recommended.
It is important for each treatment plan to consist of close monitoring, and making changes as needed based on the unique needs of each child.
ADHD effects a child’s ability to learn and develop relationships therefore effecting overall quality of life if left untreated.
How can Occupational Therapy help with ADHD?
Occupational Therapy (OT) can help children with ADHD by analyzing the unique relationship between each child, task, and environment and making modifications as needed to promote attention and self-regulation. A calming environment with decreased stimulation is optimal to maintain attention and to support self-regulation. Additional techniques to help improve the child’s attention, impulsivity, and hyperactivity may include sensorimotor strategies such as providing sensory regulating activities, using visual timers, using weighted vests or blankets, and sitting on a therapy ball chair to promote attention. Occupational Therapists can help children with ADHD develop skills related to emotional regulation, social interaction, planning, organization, attention, and behavior. In addition, they may also provide parent and family education to help families learn about ADHD and support their child across all environments.
Tips to Help Manage ADHD Symptoms
- Getting the recommended amount of sleep each night based on age
- Limiting the amount of screen time from TV, tablets, and phones each day
- Eating a healthful diet and incorporating physical activity into a daily routine
- Keeping a routine and a daily schedule. Hang the schedule in an accessible location such as on the fridge and write changes in as far in advance as possible
- Organize everyday items and keep everything in its place
- Use homework notebooks and organizers and encourage your child to write everything down
- Be clear and consistent with rules and expectations
- Give praise and rewards when rules are followed! Children with ADHD often expect and receive criticism.
- Seek professional help from an OT for emotional self regulation strategies, social skills, attention/focus tools and organization/behavior therapy.
References
Attention Deficit Hyperactivity Disorder. (2016). In The National Institute of Mental Health Resource Center. Retrieved from:
https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd/index.shtml
Attention Deficit/Hyperactivity Disorder (ADHD). (2008). In Center for Disease Control and Prevention. Retrieved from: https://www.cdc.gov/ncbddd/adhd/facts.html
Case-Smith, J., & O’Brien, J.C. (Eds.). (2015). Occupational Therapy for Children and Adolescents. St. Louis, MO: Elsevier
Chu, S., & Reynolds, F. (2007). Occupational therapy for children with attention deficit hyperactivity disorder. The British Journal of Occupational Therapy, 70(9), 372-382. DOI: 10.1177/030802260707000902
Developmental Checklist
Is your child meeting their developmental milestones?
 Skip to content
Skip to content