Month: July 2018
Evaluation Step 1: At your first appointment at ABC Pediatric Therapy, you will first meet your therapist in the waiting room. The therapist will bring you back into a small room or an area in the gym to begin your evaluation. Your evaluation will begin with your therapist asking you a few questions about your child such as his/her medical history, birth history, allergies and more.
Most importantly, your therapist will ask you the following question: What are your concerns and goals for your child to achieve by attending physical, occupational, or speech therapy? 

Evaluation Step 2: After providing information about your child, the therapist will assess your child’s strengths and weakness by asking him/her to perform a series of tasks. After assessing your child’s skills, the therapist will determine if your child needs therapy services or if he/she is on track with his/her milestone achievements. If therapy is needed, it will be recommended. For example, your child may be recommended to attend therapy one time per week for a 60-minute session. 
Designing Goals: After a need for therapy is determined, the therapist will write goals to work towards in each therapy session. As a parent, your goals for your child should be reflected in the therapist’s goals for intervention!
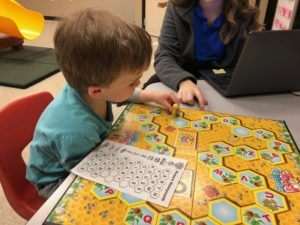
Treatment: Treatment begins day one! Treatment may take place in the large gym or a small room depending on the goal targeted and your child’s needs. The therapist will begin to work with your child to improve his/her skills and work toward meeting the goals set. Therapists love having you involved in each treatment session. This is how you learn more about how to help your child. Treatment sessions will continue until your child meets his/her goals set by you and your therapist. The more consistent you are with attending your scheduled appointments, the faster progress will be made. Goals will be updated and changed to challenge your child to progress his/her gross motor, fine motor, or speech skills.



Home Exercise Program: Beginning on your first day, your therapist will provide you with exercises or activities to perform at home for practice. Your therapist will provide guidance on how to practice the tasks to help your child be successful. Ask your therapist for tips on how to practice while keeping up with your busy, daily schedule! Your home exercise program will be updated as your child progresses through therapy.
Discharge: After your child has met the goals set and your child has overcome your concerns, your therapist will recommend discontinuing therapy services. As the parent or guardian, you will be provided with a home program to continue to practice at home. Your therapist will call you periodically to check in. If concerns arise after discharge, you can call back to meet with your therapist. Your therapist is here to help create the best life for all children!


Read More
Learning to walk is a fun and exciting time for new parents and young children. Children typically begin to walk independently around 12 months of age and require a lot of practice, trial and error, falling and getting back up. Kids do not have a normal, adult-like walking pattern until closer to the age of seven. Therefore, those who are just learning to walk or have been walking for a very short period of time will have a wider base of support with their legs further apart, absent heel strike, and absent arm-swing. It isn’t until 18-24 months of age when little ones consistently begin to land on their heels and swing their arms reciprocally. Due to this lack of heel strike, it may appear that your child is walking on their toes. Toe walking can be considered a normal variant of early walking. However, it becomes more of a concern if and when they consistently walk up on the tips of their toes.
Why is my child walking on the tips of their toes?
Many kids toe-walk and the reason is often unknown and can be considered idiopathic. Idiopathic toe-walking means there is no known reason; the child does not have any other medical diagnosis that would cause the child to walk this way. Sometimes, toe-walking can become purely habitual.
A few potential factors that may contribute to the toe-walking include: difficulty with processing sensory information through their feet and/or legs, muscular tightness and/or weakness, poor bony alignment, or nervous system involvement. Toe walking can also be associated with several diagnoses, including cerebral palsy, muscular dystrophies, autism spectrum disorder, and global developmental delay. However, this is only an association and does not mean the child has one of these conditions nor does it mean that they will necessarily toe-walk if they are diagnosed with one of these conditions.
When does toe-walking become a concern?
Toe-walking puts abnormal stresses on the body that can lead other problems. It causes extreme tightness of the calf muscles, limiting the motion of the ankle. With prolonged toe-walking, the calf muscles become tight and can limit the range of motion at the ankle. This loss of motion will not only affect the way they walk, it will make riding a bike, walking up/down stairs, and playing more difficulty. Finally, toe-walking causes more stress at the knees, hips, and back putting the child at risk for pain and/or injury in the near future.
What can be done if the child does not outgrow the toe-walking?
It is possible that the child will “outgrow” this, with the emergence of a normal heel-to-toe pattern around the age of 18-24 months. But what do you do if they don’t? Physical therapy is a great first choice of treatment to help your child beat the habit of toe walking in a conservative manner. In other words, using treatments such as stretching, strengthening, orthotics or shoe inserts, and play under the supervision of a physical therapist can help reverse the effects that toe-walking has on the body, and get your little one walking with an age-appropriate pattern. If these forms of treatments are not working as planned or the child’s toe-walking has led to severe loss of motion within their feet and ankles, another option a physical therapist can provide is called serial casting. Serial casting is considered a conservative intervention. A series of casts are used (similar to a cast you may have after breaking a bone), which is typically on for one week, and then replaced weekly for a set period of time. With each cast, the child’s foot is brought forward towards their body (dorsiflexion) in order to stretch the calf and restore motion. At the end of the casting, the goal is for the full range of motion to be restored in order to allow for a proper heel-to-toe walking pattern and eliminate the habitual toe-walking. If left unaddressed, toe walking can lead to contractures (shortening of a muscle leading to decreased movement) and the inability to stand with feet flat on the ground. As the child grows, surgery may be recommended when left unaddressed or if the severity of the toe walking is such that conservative measures are unsuccessful.
Toe-walking can be decreased and a typical walking pattern can be established. If you notice that your child consistently walks on their toes, consider making an appointment with a physical therapist in order to prevent future pain and injury, and help set up your child for future success. If you have any questions, contact ABC Pediatric Therapy, specifically a physical therapist, for more information, and visit our website at www.abcpediatrictherapy.com to find the location nearest you.
Read More I wrote the following in February 2005 when Jakob was three-and-a-half…
I wrote the following in February 2005 when Jakob was three-and-a-half…
“We got the results of Jakob’s ADOS yesterday and they weren’t what I was expecting. I really believed he would test on the autism spectrum but he didn’t. It was autism. The label is autism. To put it in perspective, his score could’ve been 0-22 with 0 being no autistic characteristics. A score of 7-12 would have been autism spectrum disorder. Jakob scored a 16. Autism.
For the first few hours after we heard that word, I felt like I was having an out-of-body experience. Thoughts were racing through my head at 100 miles-an-hour…What do I do next? What happens when we get old? What happens to Jakob when we die? Will he ever talk? Should I have another baby so he won’t be alone? What if we have another baby and he/she is autistic too? Or has something else wrong? How do we afford more therapy? What haven’t we tried to do to help him? What does he understand…does he know how much we love him? This must be my fault…what did I do to cause this? What did his dad do? Was it his vaccinations? How do I tell my family? Will they understand…will Jakob ever understand??? How will other kids treat him? HOW DO I FIX THIS???”
Reading that takes me back to the place I was in that day and I remember those feelings so clearly. Partly because they return every now and then in new and different ways. The uncertainty, the wondering, the frustration, the fear. It’s all just a part of the party, I suppose.
The big difference now is I’ve learned how to not wallow in the pain and suffering that comes with all that fear. I’ve figured out that the fear is all in my head. It’s not real. It’s all imagined. When I look at Jakob and I’m experiencing any kind of stress or discomfort about his health and well-being or his future, I ask myself one simple question, “Other than what I’m thinking and believing right now, is he ok? Am I ok?”
And so far, every single time I’ve asked that question, the answer has been that we’re both ok. Better than ok, actually, he’s happy, and for the most part, he’s healthy. For the parts that aren’t so healthy, we see some great doctors, we’re managing his symptoms and healing his system. He continues to learn and progress and he’s developed a passion for trying new things. He has so many people who love him.
Then I remind myself that I believe the universe is benevolent and that the purest of heart will always be taken care of. That one belief eases any and all concerns that may arise in me. It’s faith. It’s a knowing. It’s a matter of letting go of all the worry and being in the moment and just loving it all. What a journey. What a kid. What a life. It’s all just how it’s supposed to be. There’s nothing for me to fix. It’s all perfect.
Read MoreWhat is torticollis?
You may have noticed that your baby may prefer to look towards one side, they have difficulty turning their head towards one side, they may keep their head tipped towards a side or maybe they have a flat spot on the back or side of the head. If so, they may have something called torticollis or “wryneck”. Torticollis is tightness of neck musculature that typically causes them to tilt to one side and look towards the other. It can happen before, during, or after birth and can affect their development. It primarily causes the muscles on one side of the body to become tight with the muscles on the opposite side of the body becoming stretched and weakened. This makes it harder to look from side to side, to use their legs and arms normally, and ultimately affect the way they learn to sit, crawl, and play.
Effect on Head Shape
Sometimes prolonged positioning of the baby’s head in one direction cause a flat spot (this is called plagiocephaly). It can affect the shape of the rest of the baby’s head, with changes in the forehead (this is called bossing), changes in ear positioning, and facial asymmetries such as jaw recession. Some babies prefer to be on their backs but do not have a preference for turning their head towards one side, which could lead to the entire back side of the head is flattened (brachycephaly), making the head appear wide. Intervention by a physical therapist, education on positioning and supervised tummy time can help improve the shape of your baby’s head!
Importance of Supervised Tummy Time 
After the “Back to Sleep” program was implemented in the 1990’s, there was an increase in torticollis and head shape concerns. The program was successful and the safest place to place your child when asleep and/or unsupervised is on their backs. Many babies spend most of their awake and sleep time on their backs or in equipment such as a bouncer, a swing, a car seat, etc. With more and more time spent in these passive positions, pressure is being placed on one spot of their heads consistently, leading to a flat spot.
Encouraging the baby to look towards the other side from their preferred side will help take the pressure of their flat spot of their heads. One of the best ways to improve the shape of the head while also improving their strength is the use of tummy time while the child is supervised and awake. When a baby spends time in active floor play it encourages motor development, Tummy time especially allows them to build strength in their neck muscles. Supervised tummy time while awake is a very important part of your baby’s development! Eventually they learn how to bear weight through their forearms and extended arms, further building strength in their necks, backs, and arms. By doing so, there is less pressure on their heads and it enforces a more neutral or midline position.
How is this treated?
In many cases, traditional physical therapy can help your baby’s strength, posture, development and head shape. Treatment typically consists of is parent/caregiver education, stretching tight muscles, strengthening weak muscles, and monitoring/addressing developmental gross motor milestones (i.e rolling, crawling, and sitting). Although the physical therapist plays an important role, it is also crucial that the home exercise program be followed as well. This program typically consists of stretches, re-positioning techniques, and strengthening exercises all taught by the physical therapist and usually practiced during the session.
If your baby’s head shape does not respond to repositioning and addressing the torticollis, a cranial shaping helmet may be used to directly address the shape of your baby’s head. The use of the helmet is backed by research and has be proven to be the most effective in terms of returning the head shape towards a more normal appearance. The helmet is worn 23 hours of the day, and is changed periodically by the orthotist as they baby’s head grows.
If you have further questions about torticollis, the role of physical therapy, or the use of a helmet, contact an ABC Pediatric Therapy physical therapist for more information and to schedule an appointment. Visit our website at www.abcpediatrictherapy.com to find the nearest location near you.
Read MoreLarge Motor:
Bike or scooter riding
Jump rope
Throw, kick and catch a ball
Hit a ball with a racket or bat
Swim
Hike
Outdoor sports like kick ball, baseball, soccer
Follow a line of sidewalk chalk along a jagged and curved path.
Water balloon toss or water balloon baseball
Hopscotch
Small motor, Sensory and Motor Planning:
Sidewalk chalk
Scavenger hunt outside (find something: rough, smooth, green, pink, on top, under etc)
Obstacle course outside
Swim for balls or diving toys with sight words
Fill spray bottles with liquid watercolors, spray on easel outside with watercolor paper.
“Paint” with water, get out the old paintbrushes, paint rollers and mops along with a bucket of water and have the kids “clean” or “paint” the deck or pavement.
Paint rocks or a flower pot for the garden
Catch fireflies
Pick flowers
Make paper airplanes
Make ice cream or popsicles
Play I-Spy on road trips
Leaf rubbing
Plant flowers
Make a windsock
Language:
Swim for balls or diving toys with speech words on them
Name items that start with certain letters or sounds while taking a walk
Talk about what is on top/under/next to while running errands
Ask Who, What, When, Where questions
Describe items outside or on road trips
If you have concerns about your child’s development, go to http://checklist.abcpediatrictherapy.com and fill out this checklist about your child. You will receive tips and tricks on how you can help your child. You will also find much information at https://www.abcpediatrictherapy.com.
Read More
Intellectual skills: Provide your child with fun learning games and toys. Reading to them, pointing out things on the pages and asking questions are great ways to build language and increase interest and creativity.
Motivation to learn: Encourage your child to do their best, follow the class rules and show a genuine interest in what they are doing in school. Encourage your child to color, draw, dress themselves and wash their hands. If mom and dad are invested and interested, their kids will want to make their parents proud!
Social skills: Sharing, taking turns, trading toys, waiting turns, eye contact, speaking with an appropriate voice volume and personal space are all skills that will be needed in Kindergarten. As parents, we can guide our children in these skills when we play games and when they play with peers. Community activities provide great opportunities for kids to have fun while building social skills. Craft days at the local craft or hardware store, community sports, the local activity/community center and even a trip to the zoo can all give children experiences to build their social skills.

Behavior-management skills: Talk to your child about safety and appropriate behaviors in various settings; how to act on the playground, how to act when an adult is giving directions and how to act when working in a group all require children to use skills that need to be taught ahead of time. Provide time daily for your child to actively play and use their imagination. We can’t expect a child to behave and listen if they don’t have an outlet to play and be a kid. Simple chores can teach your child the value of taking care of things and putting things away; in school they will be expected to do these tasks on a daily basis so it needs to be a skill that is expected at home.
Readiness to learn: Encourage your child to ask questions and help them find the answers! Providing healthy food options, a sense of security, keeping a regular sleep routine, encouraging developmental skills, providing a nurturing home environment, and having parents who show excitement for learning and Kindergarten will get your child ready to learn and lessen anxiety about school!
If you need help getting your child ready for Kindergarten, let us know. We love to help! Go to https://www.abcpediatrictherapy.com for an ABC location near you.
Read More Skip to content
Skip to content